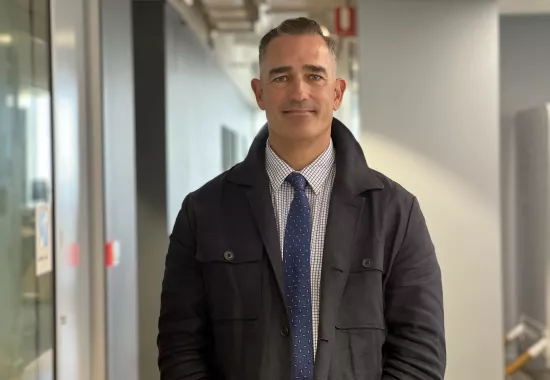
We would like to congratulate one of our emerging leaders at the Kolling Institute who has received a prestigious award at an international conference in Melbourne.
In her final year of her PhD, Caitlin Fenech has been presented with a President’s Special Commendation award at the 36th World Congress of Neuropsychopharmacology, CINP-AsCNP 2025.
Caitlin has also taken to the stage today to deliver a presentation and informative poster.
She has welcomed the experience and her encouragement award.
“Receiving recognition at an international conference is very exciting, especially as my PhD story is finishing up, and it has come out as an interesting story,” she said.
“For the award application, I sent in my abstract and a 150-word statement of the reason why I wished to be considered for the encouragement award.
“In my statement, I described my passion for neuroscience and eagerness to meet other passionate individuals studying the brain.
“My research is investigating the role of a group of neurons in the midbrain in chronic pain. We have found a novel pain circuit in the brain that controls both sensory and emotional responses and is changed following chronic pain.
“This is really exciting as these insights increase our knowledge of how pain and chronic pain are processed in the brain, and will help develop effective treatments for pain conditions in the future.
“Excitingly, the team will be submitting the data for publication in the next few months.”
Head of the Neurobiology of Pain Laboratory within the Kolling Institute, Associate Professor Karin Aubrey is thrilled Caitlin’s efforts have been recognised.
“The findings of Caitlin’s PhD project have advanced our understanding of how the brain senses pain and organises our responses to pain in normal conditions and how it changes when chronic pain develops,” she said.
“This information is essential for developing medications that address chronic pain specific dysfunctions.”
“It’s been wonderful to see a talented, emerging researcher recognised in this way.”
The international conference has brought together experts from research and medical institutions, worldwide regulatory authorities and major pharmaceutical companies.
The theme this year is Advancing Intelligent Horizons Towards Brain Health, with the presentations are focusing on pain, schizophrenia, depression and addiction.