An innovative tool which could revolutionise the detection and treatment of musculoskeletal and neurological conditions will be further developed following a $230,000 gift.
The donation was made following a campaign by the University of Sydney’s Advancement team and the NORTH Foundation to support the world’s first open-source dataset of whole-body muscle composition.
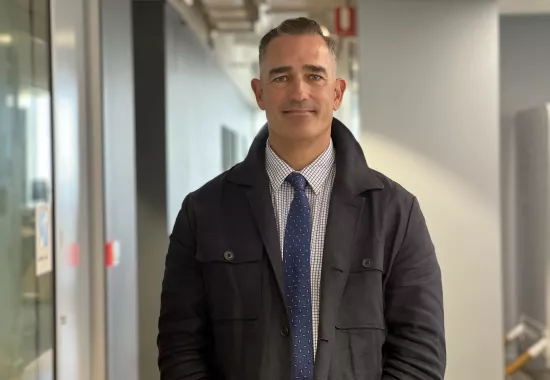
The Kolling Institute’s Academic Director Professor James Elliott said there is a critical need for the diagnostic tool with musculoskeletal and neurological conditions among the leading causes of illness and disability worldwide.
“With these conditions affecting more than four billion people, they are expected to cost around $21 billion in healthcare expenditure by 2033 in Australia alone,” he said.
“Early identification and intervention are crucial if we are to offer long-term health benefits and minimise the disease burden.
“We know that these conditions often lead to a steady decline in muscle health, and this decline is evident by an increase in fat deposits in the muscles and the loss of muscle fibres.
“CT and MRI scans can be used to identify these changes, but the time it currently takes is prohibitive.
The MuscleMap tool however, will automatically identify any changes, potentially revolutionising the detection of muscle health in any part of the body. It could inform treatment for everyone from elite athletes to astronauts and older people with complex conditions.
Astronauts for instance, experience significant muscle loss due to the effects of prolonged exposure to zero gravity.
Using existing MRI and CT scans, the landmark global study has applied an artificial intelligence model to produce a dataset of muscle health of any part of the body. This will enable a patient’s muscle deterioration to be compared with a healthy person’s.
Professor Elliott said this will mean a clinician will be able to upload a scan into the MuscleMap program, and within minutes, will have access to detailed information measuring muscle composition compared to a reference dataset.
“For athletes and the general population, the tool will accurately inform the journey from injury to repair, recovery and return to physical activity.
“For patients with osteoporosis, the program will provide a detailed analysis of overall health and muscle deterioration, which will then inform personalised strategies to develop healthier muscle mass and improve general health and wellbeing.
“We are very appreciative of this generous donation to the MuscleMap project. It will enable the broader team to continue developing the digital infrastructure needed to launch the open-source portal.
“It will be a pioneering resource, accessible to clinicians and researchers globally, and supporting the long-term health of communities.”
To donate to the innovative MuscleMap project visit the NORTH Foundation.