The key to long term weight loss and good health is not just a new, dynamic medication like Ozempic, but a much broader approach involving comprehensive support.
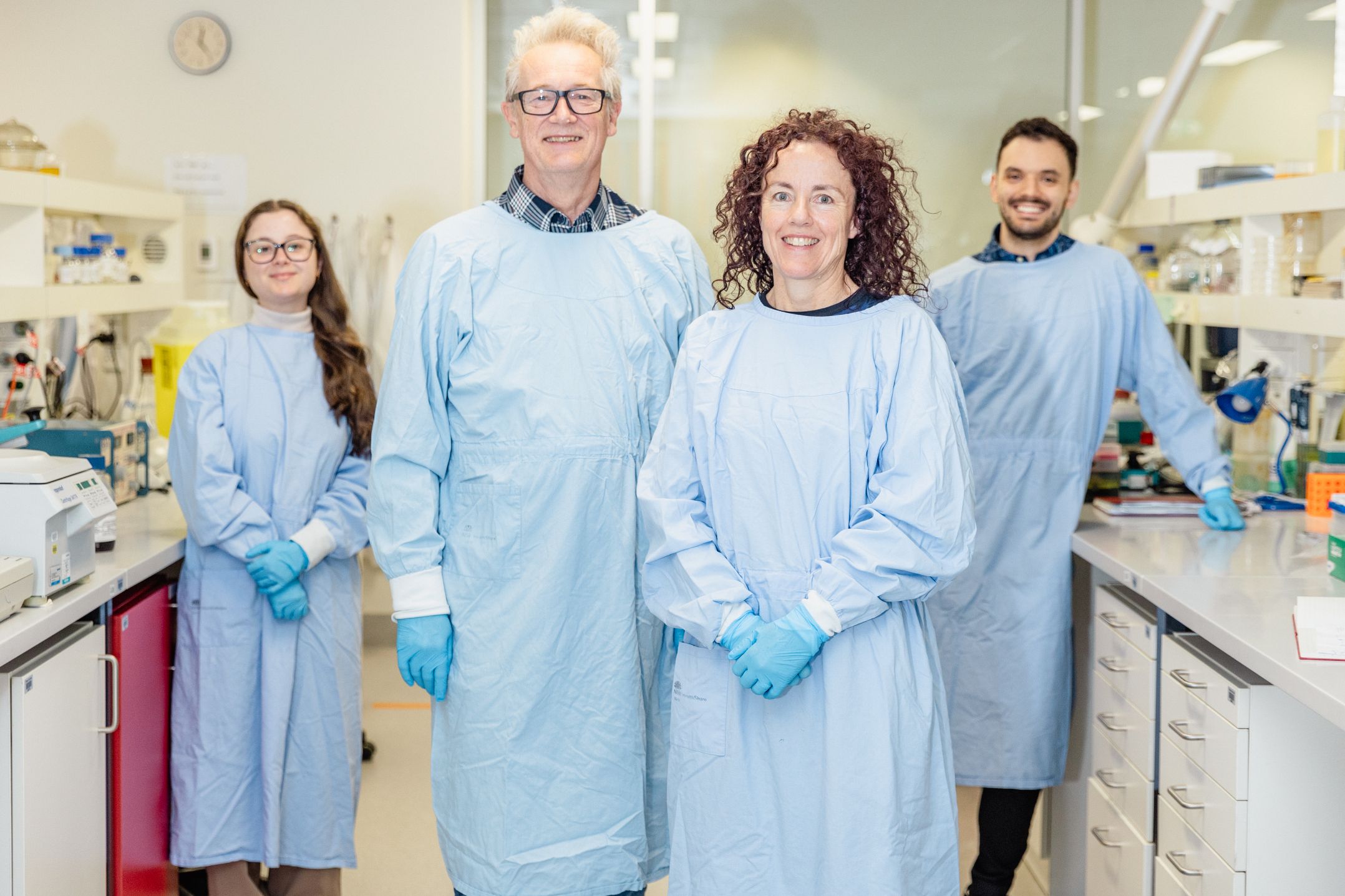
This is a view held by leading endocrinologist and senior Kolling Institute researcher Professor Sarah Glastras, who is calling for a shift away from the perception that these new game-changing medications are the only answer to complex health challenges like obesity and heart disease.
Professor Glastras is part of a growing body of health professionals advocating for a holistic approach to weight loss, involving a multi-disciplinary team including an endocrinologist, dietitian, exercise physiologist and counsellor when necessary.
New evidence is emerging around the risk of weight gain once the medication is stopped, and the potential loss of lean muscle and bone density due to the rapid weight loss.
Professor Glastras says these risks can be reduced with a tailored health program, encompassing weight training, education and healthy diet support.
“If we’re going to be able to make leaps and bounds in the space of weight management, not just for the individual, but for their family and their children, it has to be a lot more holistic than just the medication,” she said.
“I’m very much in favour of being able to access all the team players.
“Hopefully, we’ll see better wraparound care going forward, including a national approach with qualified practitioners, like exercise physiologists who can really offer patients structured and safe programs.
“We’re running a lot of clinical trials at Royal North Shore Hospital in this area, and these trials offer a good opportunity to receive greater support.”
The hospital’s Diabetes and Obesity Research team is currently seeking participants for two clinical trials focusing on long-term weight management.
One study is for adults who:
- Have obesity with a Body Mass Index (BMI) over 30, or
- Are overweight with a BMI over 27 and a health condition such as high blood pressure or prediabetes, and
- Do not have type 2 diabetes.
The second study is for adults who are overweight or obese, and using a stable weekly weight-loss injection like Ozempic, but would like to explore options for additional weight loss.
To find out more or register your interest, please contact the research team at
nslhd-endocrineresearch@health.nsw.gov.au
Professor Glastras said by taking part, you could help advance treatments for weight management and progress medical research, while also benefitting from a carefully-monitored program.