Northern Sydney Local Health District hosted the latest stop on Sydney Health Partners’ 2025 roadshow, Translation in Action.
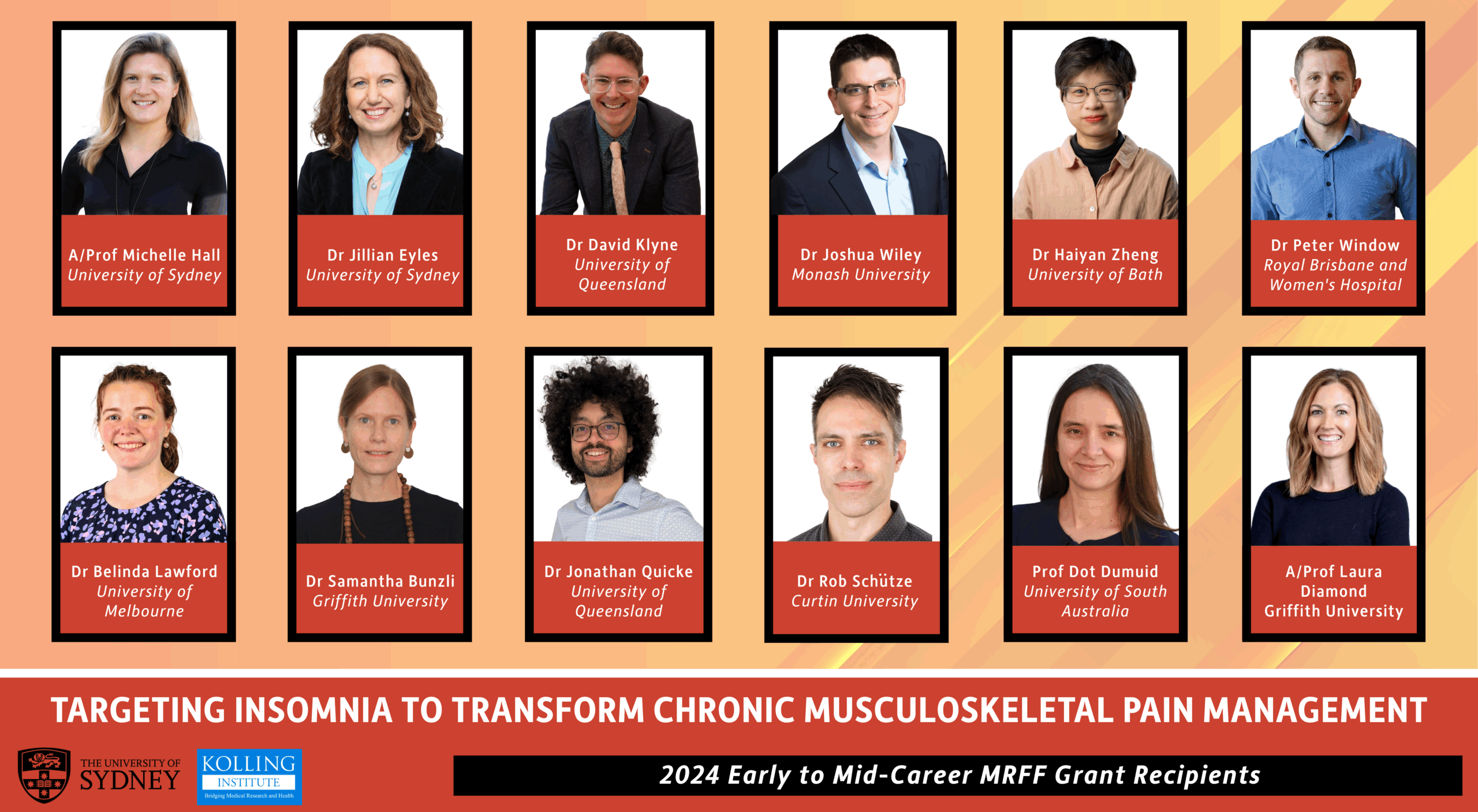
More than 70 researchers and clinicians gathered at the Kolling Institute to hear presentations by colleagues involved in translational research projects, and to see how Sydney Health Partners is assisting research translation.
The Kolling’s Academic Director Professor James Elliott said the district is proud to work with Sydney Health Partners to support the introduction of new approaches.
“By introducing these better models of care on a bigger scale, we have the potential to reach large parts of the community within our district, and to test these approaches for a much larger population,” he said.
He encouraged everyone to consider the research opportunities in their individual field.
“We know that districts with an active research culture, where research is embedded as part of clinical care, deliver better patient experiences and better long-term health outcomes.”
Acting Executive Director of Sydney Health Partners, Professor Andrew Baillie, described the research translation pipeline, from discovery to implementation.
“The truth is that some great, evidence-based, interventions never make it to the other end of the pipe,” he said. “In that sense, Sydney Health Partners can be viewed as plumbers trying to fix a leaky and complicated set of pipes, and implementation science is one of our plumbing tools.”
Leading medical oncologist Professor Stephen Clarke praised the efforts of everyone involved with SHP to embed research in the day-to-day operations of hospitals.
“It used to be that research was almost regarded as the self-indulgence that interfered with core hospital business, and I think what we’re doing now is saying it’s an essential part of health services,” he said.
Following the Roadshow NSLHD Executive Director of Research, Associate Professor Naomi Hammond said the information presented had been timely.
“What I’m seeing is that there’s more and more people coming now to ask what they can do to get research happening in their area,” she said.
“I think this is where Sydney HealthPartners comes in: an expert research group that can support clinician researchers to bring research into their practice.”