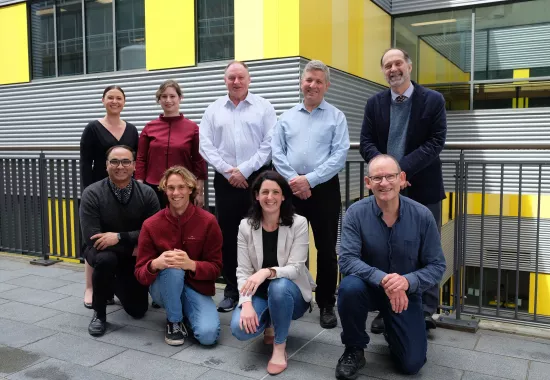
A new study by researchers at the Kolling Institute, in collaboration with the Microbiome Research Centre, has shown that multiple medication use impacts gut microbiome, and may influence the ageing process.
Gizem Gemikonakli, a PhD student at the University of Sydney, said their findings followed a longitudinal, in vivo study.
“Interestingly, mice that were given a regimen of five therapeutic medications from middle-age experienced more functional deficits as they grew older, and their gut microbiome was different to mice not taking the medications,” she said.
“This project represents an important step towards broadening our knowledge of the interaction between medications, microbiome and the ageing process.
“The microbiome is a developing area of research and we don’t quite know what a healthy microbiome looks like.
“We do know however, that microbiome affects a wide range of body functions, and is affected by diet, lifestyle factors, disease and medications.”
In a previous study published on the same cohort of mice, the Kolling researchers showed that the multiple medication or polypharmacy treatment increased frailty among the mice.
Gizem explained that like other studies, we found the diversity of the microbiome was associated with functional measures, including frailty and activities of daily living in mice.
“However, in our case it is likely the polypharmacy medications were driving both the microbiome effects and the functional deficits.”
At 21 months, which is old age, half of the mice had the medications withdrawn, and their microbiome was collected again three months later. Taking these mice off the multiple medication regimen reversed the changes that initially occurred when they started treatment.
The microbiome however did not recover completely. It was different compared to its composition before starting the medications, and also different to the mice at the same age which were not given any medications throughout the study.
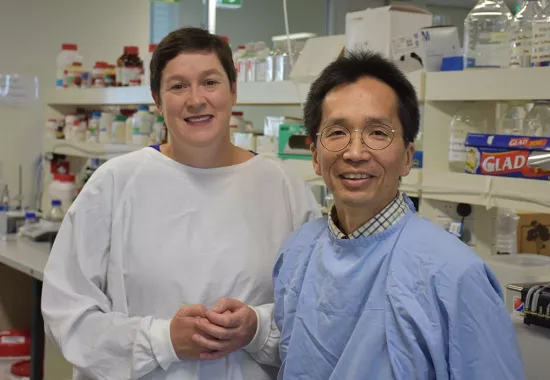
Professor Sarah Hilmer, Gizem’s supervisor at the Kolling said the two-way interactions between the gut microbiota and medications are very complex.
“Our translational study describes effects of one high risk polypharmacy regimen on the microbiome, and its partial reversibility with de-prescribing,” she said.
“This opens up exciting avenues for further research, including understanding the effects of different drugs on the microbiome and understanding how the microbiota impact on drug effects.
“Differences in microbiome might explain why some people respond better than others to polypharmacy.”